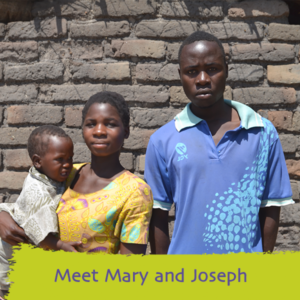
This is the beginning of the story of Mary and Joseph Chimwanza from a remote village in rural Zomba, Malawi. It is a story of how conditions in some areas of the world makes childbirth life-threatening both for mother and child. However, it is also a story of how help and kindness from strangers can save lives and inspire us.
‘On our way to hospital, we met some people who were coming from the beer hole. We become scared and because of my condition, we decided to face them and explained our story – that we were rushing to the hospital for delivery. The men then decided to escort us to the health centre.’
‘Later in our discussions with the men, we discovered that two of them belonged to the Participatory Learning Action (PLA) group in our village.’
In 2015, Maternity Worldwide introduced a project on improving maternal and newborn health to 80 villages in the Zomba region where Mary and Joseph Chimwanza live. As part of the project, Maternity Worldwide introduced Participatory Learning Action (PLA) activities to women’s groups in 80 villages in Zomba. At the meetings, participating women and men are educated about how women remain safe during pregnancy, about the danger signs of pregnancy and when should they seek help.
‘My condition become worse when it started to rain and it was cold. One of the men who joined us had a raincoat which he gave me and we had to seek shelter in the nearby village until the rain became less heavy. When the rain stopped, we continued our journey to the hospital where we were assisted quickly and it did not take long before I delivered our baby, Earnest. My husband was overwhelmed to learn that the men who helped us were part of the PLA Group and he was encouraged to join the PLA group in our village where he is still a member.’
‘As a small family, we are very grateful to Maternity Worldwide for having introduced the PLA to the women’s group in our village’
‘As a small family, we are very grateful to Maternity Worldwide for having introduced the PLA to the women’s group in our village and most especially that men should be part of it. If it were not for those men being part of the ‘women’s group’ it would have been very difficult for them to understand what I was going through as a first-time mother and difficult for my husband to realise the importance of being part of the group in our village.’
As Mary re-tells her story with baby Earnest in her arms, it is testament to the benefits of the Maternity Worldwide project. Mary and Joseph knew the importance of giving birth in a hospital and managed to get to the health centre safely, where they were met by a team of skilled medical personnel ready for delivery.


 This was Qiybise’s fourth pregnancy. She had safely delivered each of her previous babies at home and was planning to do the same this time. The skilled Maternity Worldwide volunteer who was running the clinic assessed Qiybise to see if there were any factors in her pregnancy which would increase her risk. She also carried out an ultrasound using a small, portable scanning machine. This showed Qiybise had a very low lying placenta (after-birth) and which was extending across the cervix (the birth canal). This means the mother is at high risk as once labour begins the baby’s head descends and pushes against the placenta. This tears the placenta from the uterus and can cause the woman to bleed profusely. Haemorrhaging in such situations is a leading cause of death in childbirth.
This was Qiybise’s fourth pregnancy. She had safely delivered each of her previous babies at home and was planning to do the same this time. The skilled Maternity Worldwide volunteer who was running the clinic assessed Qiybise to see if there were any factors in her pregnancy which would increase her risk. She also carried out an ultrasound using a small, portable scanning machine. This showed Qiybise had a very low lying placenta (after-birth) and which was extending across the cervix (the birth canal). This means the mother is at high risk as once labour begins the baby’s head descends and pushes against the placenta. This tears the placenta from the uterus and can cause the woman to bleed profusely. Haemorrhaging in such situations is a leading cause of death in childbirth.  Chaltu came to our maternal health risk assessment clinic at Ganji when she was 34 weeks pregnant. Her last pregnancy had ended in a stillbirth at home and, even though it was a two hour walk from her village, she was intending to come to the health clinic for this delivery. Chaltu was surprised to be told that she was in fact expecting twins. In rural Ethiopia childbirth can be hazardous and even more so when twins are expected. Without the support of a skilled midwife or doctor at time of delivery, babies can die as a result of long and obstructed labour and the mother’s life can also be at risk.
Chaltu came to our maternal health risk assessment clinic at Ganji when she was 34 weeks pregnant. Her last pregnancy had ended in a stillbirth at home and, even though it was a two hour walk from her village, she was intending to come to the health clinic for this delivery. Chaltu was surprised to be told that she was in fact expecting twins. In rural Ethiopia childbirth can be hazardous and even more so when twins are expected. Without the support of a skilled midwife or doctor at time of delivery, babies can die as a result of long and obstructed labour and the mother’s life can also be at risk. Burane is a young woman of 25 who lives in a small village in the West Wollega area of Ethiopia. Her village is almost two hours walk from the nearest health centre.
Burane is a young woman of 25 who lives in a small village in the West Wollega area of Ethiopia. Her village is almost two hours walk from the nearest health centre. Bultu is a 32 year old woman who lives in a remote village in the West Wollega region of Ethiopia. Her village is almost 2 hours walk from the nearest health centre.
Bultu is a 32 year old woman who lives in a remote village in the West Wollega region of Ethiopia. Her village is almost 2 hours walk from the nearest health centre. Alemi, who is 25 years old, arrived at our maternal health risk assessment clinic with very swollen ankles. We found she had high blood pressure, a potentially life-threatening complication in pregnancy. She had been pregnant twice before but on both occasions, the baby died near to the time of delivery.
Alemi, who is 25 years old, arrived at our maternal health risk assessment clinic with very swollen ankles. We found she had high blood pressure, a potentially life-threatening complication in pregnancy. She had been pregnant twice before but on both occasions, the baby died near to the time of delivery. Ayantu is a 20 year old woman who lives in a small village in the West Wollega area of Ethiopia. From her village it is almost two hours walk to the nearest health centre. The long distances involved is just one of a number of reasons why the vast majority of women in rural Ethiopia don’t attend a health clinic for ante natal care and give birth at home without being able to access skilled help from a midwife or doctor.
Ayantu is a 20 year old woman who lives in a small village in the West Wollega area of Ethiopia. From her village it is almost two hours walk to the nearest health centre. The long distances involved is just one of a number of reasons why the vast majority of women in rural Ethiopia don’t attend a health clinic for ante natal care and give birth at home without being able to access skilled help from a midwife or doctor. Aster successfully gave birth to her fifth baby at home with just her mother to help. Initially the birth seemed to have gone well and Aster delivered a healthy baby girl of 3.5 kg. But the afterbirth (the placenta) would not come out and Aster started to lose a large volume of blood. Her family carried her to the hospital but by the time they got there Aster was unconscious. She also had a seizure, which may have been due to her having high blood pressure, a recognised complication of pregnancy.
Aster successfully gave birth to her fifth baby at home with just her mother to help. Initially the birth seemed to have gone well and Aster delivered a healthy baby girl of 3.5 kg. But the afterbirth (the placenta) would not come out and Aster started to lose a large volume of blood. Her family carried her to the hospital but by the time they got there Aster was unconscious. She also had a seizure, which may have been due to her having high blood pressure, a recognised complication of pregnancy. At Maternity Worldwide we know that one of the key factors in ensuring sustainable improvements to maternal health services is that local clinical staff develop the knowledge and skills to enable them to carry out the procedures needed to save mothers’ lives.
At Maternity Worldwide we know that one of the key factors in ensuring sustainable improvements to maternal health services is that local clinical staff develop the knowledge and skills to enable them to carry out the procedures needed to save mothers’ lives.